Made possible by
Showing Up For Me and You
Mental Wellness Patch Program
for Seniors and Ambassadors
Facilitator Guide
Showing Up For Me and You Facilitator Guide | 2
Mental Health Disclaimer
The contents of the Mental Wellness Patch Program for
Seniors and Ambassadors: Showing Up For Me and You is
for informational purposes only. This program was made in
partnership with the HCA Healthcare Foundation and the
National Alliance on Mental Illness (NAMI). The information
presented by this program is not an attempt by Girl Scouts
of the USA (“GSUSA”) to practice medicine or to give specic
medical advice, including, without limitation, advice concerning
the topic of mental health. Therefore, the information from
this program should not replace consultation with your doctor
or other qualied mental health providers and/or specialists.
Never disregard, avoid, or delay obtaining advice from your
licensed mental health care provider because of something you
have read or experienced through our program. If you believe
you or another individual is suffering a mental health crisis or
other medical emergency, contact your doctor immediately, seek
medical attention immediately in an emergency room, or call 911
or 988 (the Suicide & Crisis Lifeline).
© 2023 Girl Scouts of the United States of America (GSUSA). All rights reserved. Not for commercial use. This material
is proprietary to GSUSA and may be used, reproduced, and distributed exclusively by GSUSA staff, councils, Girl Scout
volunteers, service units, and/or troops solely in connection with Girl Scouting.
Showing Up For Me and You Facilitator Guide | 3
Table of Contents
Introduction ................................................................................................................................. 4
Mental Wellness Tips for Facilitators ....................................................................................... 5
Planning and Preparation ...........................................................................................................7
Facilitation Script and Activity Guide ..................................................................................... 10
Next Steps ................................................................................................................................... 20
For Facilitators: Customizable Invitation Email
to Parents/Caregivers ...........................................................................................................21
For Facilitators: Customizable Post-Event Email to Parents/Caregivers ....................... 22
Meeting Aids .............................................................................................................................. 23
For Facilitators: Mental Health Terms to Know
For Facilitators: Symptoms of Mental Health Conditions
For Facilitators: What to Know About Identity, Culture, and Mental Health
For Facilitators: Girl Scout Safety Activity Checkpoints
—Overall Health, Well-Being, and Inclusivity
For Seniors and Ambassadors: Symptoms of Mental Health Conditions
For Seniors and Ambassadors: Your Language Matters
For Seniors and Ambassadors: Getting the Right Start
For Seniors and Ambassadors: How to Help a Friend
For Seniors and Ambassadors: Active Listening Checklist

Showing Up For Me and You Facilitator Guide | 4
Girl Scouts of the USA (GSUSA) has made a commitment
to support mental wellness for every Girl Scout because
we recognize that young people are currently facing a
mental health crisis. They are more likely than ever before
to attempt suicide, commit self-harm, and suffer from
depression and anxiety. And yet, people continue to be
uncomfortable discussing these issues. This discomfort
can be driven by the stigma often associated with mental
health issues. GSUSA wants to help start the conversation
and give Girl Scouts tools and support to better understand
and care for their mental health.
Mental health encompasses emotional and psychological
health—it impacts how we think, feel, and act. Everyone
has a state of mental health, just as everyone has a state
of physical health. Our mental health may include a
condition, such as depression or anorexia. Such a condition
can be permanent or temporary. It can be based on our
environment (such as attending online school due to the
COVID-19 pandemic) or on our response to life events.
It’s important to remember, though, that a person can
experience poor mental health without the diagnosis of a
mental health condition. Mental wellness refers to how we
take care of our mental health. It includes all the things we
might do to help realize our potential, cope with stress, and
productively contribute to our community.
What Is the “Showing Up For Me and You” Patch
Program for Seniors and Ambassadors?
GSUSA developed the Mental Wellness Patch Program
for Seniors and Ambassadors: Showing Up For Me
and You to equip high school Girl Scouts with tactics for
practicing self-care, coping with difcult situations, and
helping themselves and others. We show facilitators how
to deal with questions and concerns, and offer participants
the resources to explore, share, and reect from a space
where they can hang out and be themselves.
The Showing Up For Me and You Patch Program for Seniors
and Ambassadors was created in collaboration with experts
at the National Alliance on Mental Illness (NAMI), the
nation’s largest grassroots mental health organization
dedicated to building better lives for the millions of
Americans affected by mental illness. We received
additional input from an advisory group made up of mental
health professionals and Girl Scout council leaders.
The Showing Up For Me and You Patch Program for
Seniors and Ambassadors was generously funded by the
HCA Healthcare Foundation, whose mission is to promote
health and well-being and make a positive impact in all
the communities served by HCA Healthcare, one of the
nation’s leading providers of healthcare services. Thanks to
HCA Healthcare Foundation’s support, GSUSA is working
toward the larger goals of destigmatizing mental illness,
normalizing conversations around mental health and
mental illness, and delivering inclusive programs for
Girl Scouts of all backgrounds.
Introduction
Mental Wellness—Why Now?

Showing Up For Me and You Facilitator Guide | 5
Mental Wellness Tips for Facilitators
Creating a supportive environment is especially important for a mental wellness program. Here are best practices
and tips to help make this a meaningful experience for everyone.
● Mental health can be a difcult topic to discuss with
young people. It’s impossible to know everything
about their lives and how certain topics in this Mental
Wellness Patch Program will affect them. Give them
permission to stop or skip an activity if they don’t
feel comfortable. This is where having more than one
volunteer will come in handy.
● When a topic comes up that you don’t feel equipped
to address, let Seniors and Ambassadors know you’re
putting it in the “parking lot.” This means you’ll be
parking the issue for now. Write it down so you can
follow up later. This gives you the time to get more
information if needed. Parking lots are also helpful if you
run out of time to discuss something. Write the topic on
a large piece of paper to revisit either later in the program
or at another meeting. Preparing yourself to come back
to parking lot items builds trust with the group.
● Let Seniors and Ambassadors know that
condentiality is key. However, if you hear or see
something you need to share about a Senior or
Ambassador, contact your council for guidance.
The meeting aid Girl Scout Safety Activity
Checkpoints—Overall Health, Well-Being, and
Inclusivity (p. 31) also provides guidelines for
addressing and reporting mental health concerns
about a Girl Scout.
● Tell participants they can share or not, depending on
how they feel. Everyone has different experiences,
comfort levels, and abilities to discuss a topic, and
there should be no pressure on anyone to share.
However, if you notice one or two participants doing
most of the talking, you can redirect the conversation
by saying:
• “Yes, I see where you’re going with that. I’d love to
hear thoughts from other people in the group.”
• “Let’s pause for just a moment to allow the entire
group to reect on or respond to what you said.”
• “Thanks for sharing! What do other people
think?”
● Encourage participants to speak up if they hear a
hurtful comment or would like to recognize and repair
something that may have hurt someone else. Even
when someone means well, they can still say things
that might negatively impact others. Taking a moment
to recognize when something we said has hurt
someone helps to strengthen our friendships.
The subjects of mental wellness and mental health can be delicate—
you’re not expected to be an expert or have all the answers.
Maintain a Girl Scout-led environment.
Showing Up For Me and You Facilitator Guide | 6
● Use person-rst language. A person isn’t dened
by a condition and shouldn’t be addressed as such.
A person experiences bipolar disorder—they aren’t
bipolar. A person experiences mental illness—they
don’t belong to a group called “the mentally ill.”
● Be open to “checking” the group’s stigmatizing
language. Challenge misconceptions. If you hear
someone use harmful language, let them know. For
instance, words like “crazy” or “insane” reinforce the
idea that mental health conditions are extreme, rather
than the reality that they are quite common. Instead,
we should say things like, “someone with a mental
health condition” or “someone who has depression.”
● Don’t use mental health conditions as adjectives.
A person shouldn’t say they have “OCD” because they
like to organize or say the weather is “bipolar” because
it keeps changing. Doing this minimizes the actual
lived experiences of people who have mental health
conditions.
● Be cautious when talking about suicide. Suicide
is a sensitive topic and should be discussed in a way
that is respectful to the person and their loved ones.
A person is “lost to suicide” or “died by suicide” rather
than “committed suicide.” If a person tries to take their
life, they “attempted suicide” as opposed to “had an
unsuccessful suicide.” Make sure Girl Scouts aren’t
speaking about suicide in a casual way (i.e., “That test
was so hard, I wanted to kill myself”); suicidal ideation
shouldn’t be treated lightly.
● Avoid the terms “others” or “abnormal.” Referring
to people experiencing mental illness as “others” or
“abnormal” creates an “us versus them” narrative.
This can make people with mental illness seem inferior
and as though they’re the outliers of society—which
they aren’t.
● Avoid talking about or labeling feelings as good or
bad, positive or negative, normal or not normal.
Think of emotions as information we pay attention to
and learn from.
Finally, make sure to listen and reect. Reecting is an intentional, purposeful time to examine, ask questions,
and think about an activity or experience. After each section of the program, engage in reection. It helps
participants move forward with a deeper understanding of what they learned.
Help the group understand the importance of the language we use to
discuss mental health. Words are powerful; they can both heal and
harm. Using language that is respectful, accurate, and empathetic
helps to break the stigma related to mental health conditions.
Mental Wellness Tips for Facilitators

Showing Up For Me and You Facilitator Guide | 7
Planning and Preparation
Take these steps to plan and prepare. Remember, this program is designed for
Seniors and Ambassadors and not intended to be a multi-troop experience.
● Read through this guide to familiarize yourself
with the content, including facilitation tips and
suggestions, scripts and activity guides, and
meeting aids.
● Carefully review the following meeting aids for
facilitators:
• Mental Health Terms to Know and Symptoms
of Mental Health Conditions to learn the proper
vocabulary and denitions so you can use them
correctly and consistently.
• What to Know About Identity, Culture, and
Mental Health to understand how identity and
cultural background can affect responses to
mental health issues and access to treatment
in different communities. This information may
apply to participants.
• Girl Scout Safety Activity Checkpoints—
Overall Health, Well-Being, and Inclusivity
to see guidelines for addressing and reporting
mental health concerns about a Girl Scout.
Contact your council for additional guidance
or to obtain the full version of Safety
Activity Checkpoints.
• Your Language Matters: You’ll give this meeting
aid to participants during Activity 2 (p. 14), but
you can also keep a copy with you to reference as
needed. If anyone uses stigmatizing language at
any point, you can gently say: “Remember, saying
_______________ can be stigmatizing to people
with mental health conditions. Instead, let’s say
__________.”
● Take the “The Mental Wellness Patch Program:
Why It Matters and How to Implement It” course
in gsLearn (required):
• “The Mental Wellness Patch Program: Why It
Matters and How to Implement It” (approximately
20 minutes) allows you to learn more about
mental health conditions and how they affect
the group you’ll be working with. We never know
what others are going through, so being prepared
for sensitive topics and big emotions will help you
feel more condent in facilitating the Showing Up
For Me and You Patch Program for Seniors and
Ambassadors.
● Take two gsLearn courses that provide additional
support for leading the Showing Up For Me and
You Patch Program for Seniors and Ambassadors
(strongly encouraged):
• “GSUSA Mental Wellness 101” (approximately 35
minutes) offers a foundational understanding of
mental health and social-emotional development
stages, as well as tools to support the Girl Scouts
you work with. (Note, however, that it isn’t a
specic training for delivering the Showing Up
For Me and You Patch Program for Seniors and
Ambassadors.)
• “GSUSA Delivering Inclusive Program”
(approximately 20 minutes) lets you practice
using inclusive and equitable language to support
the identities of all Girl Scouts and foster a
cohesive environment.

Showing Up For Me and You Facilitator Guide | 8
● Decide on a location and plan your setting. You can
hold the Showing Up For Me and You Patch Program
for Seniors and Ambassadors as an in-person troop
meeting or a council or service unit event.
For an in-person troop meeting:
• We recommend having a group of no more
than ten Seniors and Ambassadors.
• To accommodate a larger troop, you could
consider splitting into two groups, with at least
one facilitator overseeing each. Use additional
volunteers to help facilitate as needed.
• Create a relaxing space that’s quiet and cozy
for the group. Think about pillows or sitting on
a comfortable rug or chairs.
• Nature is nurturing. If possible, consider
meeting outdoors, somewhere quiet
and private.
For a council or service unit event:
• Reserve a location in advance.
• Send out information to participants at least
two weeks before with relevant information
about time, location, and parking. Send
reminders up to the day.
• At the event, divide Seniors and Ambassadors
into groups of no more than ten. Have at least
one facilitator for each group; use additional
facilitators as needed.
● Recruit mental wellness experts and other
volunteers to help facilitate.
• To the extent possible, bring in experts and
volunteers who reect the community of Girl
Scouts they’ll be supporting.
• Talk to your council and friends and family
network about relationships they might have
with mental wellness experts and professionals to
help with support. For example, reach out to your
local NAMI afliate to see if they can help you
nd volunteers. (Note: It may be best not to invite
a professional who provides services to one of the
Girl Scouts in your group, since that may impact
the participation of the Girl Scout and can lead to
a breach of condentiality.)
• Enlist other volunteers to help facilitate breakout
groups as needed.
● Reach out to participants and their families or
caregivers in advance.
• Send an invitation for Seniors and Ambassadors
to take part. (See the Customizable Invitation
Email to Parents/Caregivers meeting aid p. 21.)
• Assure them this will be a comfortable space for
participants to learn about mental wellness. It’s
possible that families may want to opt out, and
that’s okay, too.
• If you’re hosting Showing Up For Me and You
Patch Program for Seniors and Ambassadors is
in a different location than your regular troop
meetings, make sure to provide the address
and directions.
● Gather and print out activity materials and
meeting aids for Seniors and Ambassadors.
• Read through the materials list in the “Showing
Up For Me and You Patch Program for Seniors
and Ambassadors at a Glance” chart on page 9 to
know what specic items you’ll need and what to
prepare ahead.
• View NAMI’s short video Ending the Silence
before showing it to the group, so you’re prepared
to lead the discussion during Activity 1 (p. 12). It
goes over the ten most common signs of a mental
health condition.
● Be prepared to accommodate the age differences
or maturity levels in your group. Experience and
maturity levels can vary among 9th to 12th graders
(14- to 18-year-olds). You know your group best.
Read through the activities and decide if you want
to separate participants into smaller teams by age.
Keep in mind, though, that it can be valuable to
group younger participants with older ones to share
experiences.
• Think about what you are personally willing
to share. Participants might not always be
comfortable initiating or contributing to the
conversation. Hearing from you could give them
more condence to share their own experiences.
For example, you might say, “I was really sad
when I found out that my best friend was moving
to another state.”
Planning and Preparation
Showing Up For Me and You Facilitator Guide | 9
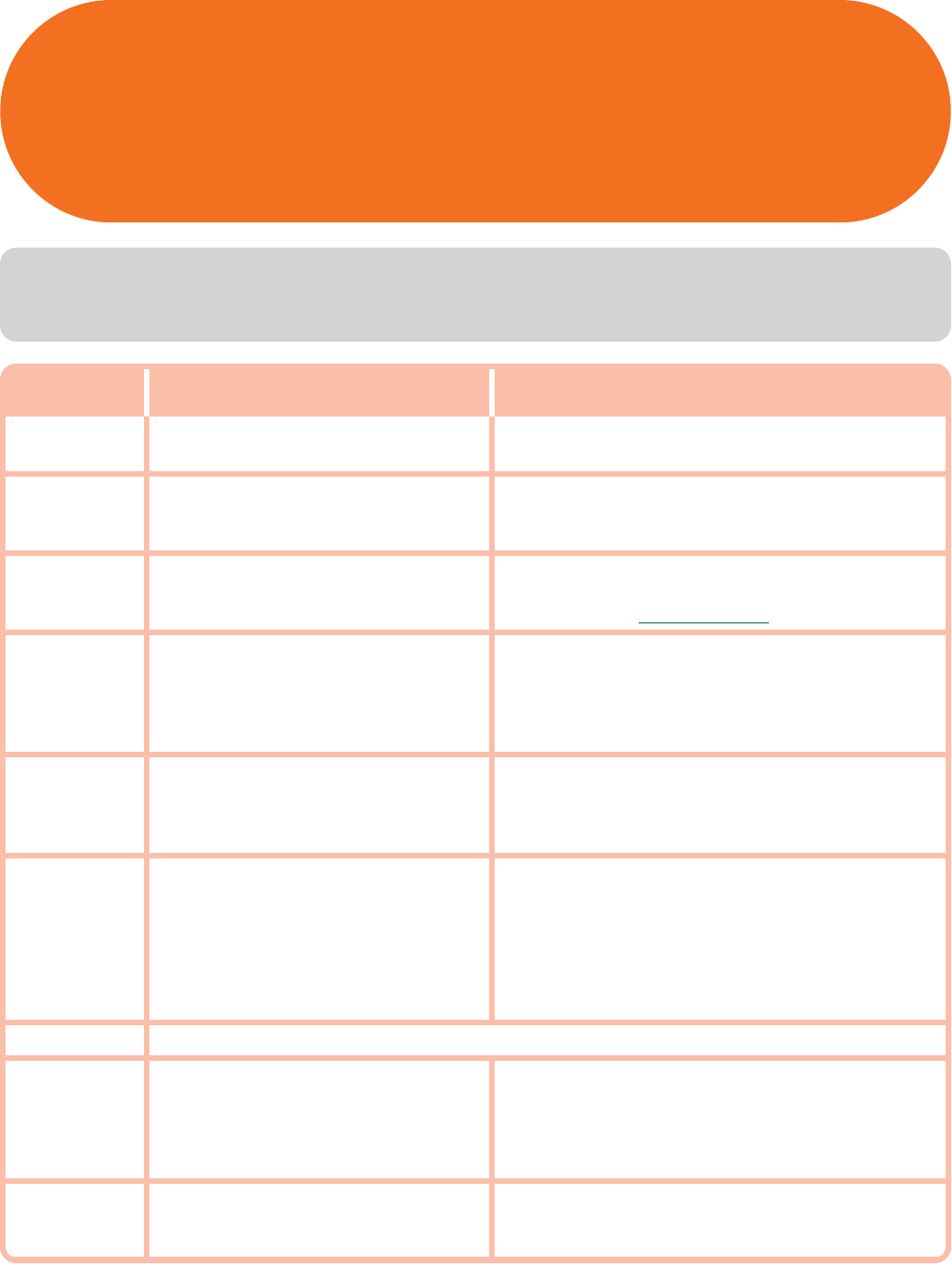
Time Activity Materials
5 minutes
As Girl Scouts Arrive:
Mental Health—What Comes to Mind?
• Paper
• Pencils or pens
10–15 minutes
Introduction to the Showing Up For Me
and You Patch Program for Seniors and
Ambassadors
• Markers
• Whiteboard or large piece of paper with an easel
10–15 minutes Activity 1: What Is Mental Health?
• Symptoms of Mental Health Conditions meeting aid
(one for each participant)
• Device to show Ending the Silence video
15 minutes Activity 2: Language Matters
• Your Language Matters meeting aid (one for
each participant)
• Recording devices, such as smartphones (optional)
• Pencils or pens
• Paper
10 minutes Stretch-and-Snack Break
• Nutritious snack items such as fresh fruit, trail mix,
granola bars, and water
• Paper plates and cups
• Disposable utensils
15 minutes Activity 3: Building Resilience
• Paper (enough for everyone)
• Pencils or pens
• Large construction paper (enough for everyone)
• Small sticky notes
• Markers
• Getting the Right Start meeting aid
(one for each participant)
5 minutes Stretch Break
15 minutes Activity 4: Supporting Others
• How to Help a Friend meeting aid (one for each
participant)
• Active Listening Checklist meeting aid (one for
each participant)
• Pencils or pens
5–10 minutes Reection and Wrap-up
• Suggestion box
• Paper
• Pencils or pens
Program at a Glance
*These suggested times total 90 to 105 minutes (1 ⁄ hour).
Please adjust as you see t for your group.

Showing Up For Me and You Facilitator Guide | 10
● This Showing Up For Me and You Patch Program for Seniors and Ambassadors is designed to take 90 to 105 minutes
(1 ⁄ hours). Feel free to use another meeting to cover anything you don’t have time for.
● Start activities with the whole group before breaking out into smaller groups.
● You’ll nd suggested talking points under the heading “SAY.” Follow them as written or use them as a guide to share the
information in your own words.
Materials: Paper, pens
Purpose: Participants record their rst impressions of mental health.
Give everyone a piece of paper and have them write words or phrases they think of when they hear the term “mental health.” They
can write as much or as little as they want. Make sure they know there are no right or wrong answers. Have them fold their paper
and set it aside. They’ll look at it again at the ending reection period.
Facilitation Script and Activity Guide
Notes to Facilitators:
As Girl Scouts Arrive: Mental Health—What Comes to Mind? (5 minutes)

Showing Up For Me and You Facilitator Guide | 11
Facilitation Script and Activity Guide
Materials: Markers, whiteboard or large piece of paper with
an easel
Purpose: Participants start to learn about mental health and
mental wellness, do an icebreaker to see what experiences and
feelings they all have in common, and discuss how to create a
comfortable space for sharing.
SAY:
● Welcome to today’s Mental Wellness Patch Program for
Seniors and Ambassadors called “Showing Up For Me
and You.” I’m glad you’re here with me to explore mental
health and wellness.
● Please remember I am not a mental health professional.
There may be questions that I can’t answer or can only
answer with my own unique experience. Anything that
is left unanswered, I will work with our council to get
information and report back at a later date.
● What do you all think the difference is between mental
health and mental wellness? (Give time to respond.)
● Mental health is your emotional and psychological health.
Just like we all have a state of physical health, we all
have a state of mental health.
● We should be sensitive to how we deal with mental health
challenges because we might not know what other people
in the room are facing, which is okay! We are here to
discuss it, learn together, and support each other.
● If you have any discomfort about anything we talk about
or do, you can choose not to participate in the discussion
or activity and it’s perfectly ne.
● When you practice mental wellness, you do things to
support your mental health, like getting more sleep,
learning how to cope with stress, and nding ways to get
and give help when it’s needed.
● The goal is to give you tools to take care of yourself, ask
for help, and support others.
● And we’re going to get to all of that in just a bit. But rst,
has anyone played “Have You Ever?” (Give them time to
respond and describe the game they’ve played.)
● It’s a game where you’ll nd out more about each other by
responding to questions.
Have the group sit in a circle. Ask the following “Have you
ever…?” questions one at a time. Have group members
decide on a movement they’ll make to indicate that they’ve
done that thing or can relate to it. For example, they can
stand or raise their hand or nger. They can share the story
behind their responses if they want.
You’re encouraged to join the circle and respond along with
the rest of the group. You may nd it helpful to share a
couple of your own experiences to start the conversation or
keep it going.
Have you ever…?
● stopped being friends with someone because you
didn’t have the same interests any more
● felt left out of a group
● felt sad because someone you liked didn’t like you back
● gone outside or to your room to “blow off steam” when
feeling angry—OR—gotten mad and surprised yourself
with how angry you were
● asked for help with a personal problem
● had nights where it’s hard to sleep
● meditated
● written down thoughts to calm your mind
● felt pressured by a friend to do something you didn’t
want to do
SAY:
● What did you learn about yourself and each other?
(Give time to respond.)
● What did you notice that you had in common with each
other? (For example, maybe several have practiced
meditation or experienced sleepless nights.)
● Isn’t it amazing how common a lot of our experiences and
feelings are? But we don’t always realize that because we
may not feel comfortable talking openly about them.
● We want this to be a comfortable space where we can have
those conversations. Creating that kind of space, where
everyone feels able to participate and share, will make the
experience more meaningful and productive for all of us.
● How can we do that? Call out your suggestions and I’ll
write them down.
Introduction to the Showing Up For Me and You Patch Program
for Seniors and Ambassadors (10–15 minutes)

Showing Up For Me and You Facilitator Guide | 12
As the group comes up with their ideas, write them on a
whiteboard or large piece of paper on an easel that can be
kept in the meeting space where everyone can refer to it.
If needed, suggest the following:
● Use a signal when you want to share or add to the
conversation.
● Use “I” statements—focus on sharing your own
experience, not someone else’s.
● Encourage kindness and openness.
● Be respectful and sensitive when responding or
making statements.
● Keep the things you hear today condential. What’s
said here stays here.
● Think before you respond.
● Give everyone a chance to talk. Don’t talk over each
other.
● Make this a judgment-free zone. Everyone’s experience
is valid and important.
SAY:
● This is great! I’m going to keep this list up here at the
front of the room for us to refer to and keep in mind today.
● Like you, I’ll keep what I hear today condential.
However, if I hear certain things that should not be
kept secret because someone is at risk—for example, if
someone is harming themselves—I may need to consult
with a trusted adult to protect you.
● Now, let’s get started.
TIP: If at any point you nd the Seniors and Ambassadors
not respecting these norms, be sure to go back to this list.
Facilitation Script and Activity Guide
Activity 1: What Is Mental Health? (10–15 minutes)
Materials:
● Symptoms of Mental Health Conditions meeting aid
(one for each participant)
● Device to show Ending the Silence video
Purpose: Participants learn about mental health conditions
and explore warning signs and symptoms.
SAY:
● Call out some mental health conditions you’ve heard of.
(Give time to respond. If needed, offer examples such
as depression, bipolar disorder, obsessive-compulsive
disorder, anxiety, ADHD, and schizophrenia.)
● What do you know about mental health conditions? (Give
time to respond. If needed, say that mental health
conditions affect how we think, feel, and act; they’re
common and treatable; they’re not anyone’s fault
or something to be ashamed of. If someone states
incorrect information, try to correct it in the moment,
or say that it’s not quite accurate and put it in the
parking lot to address later.)
● Now we’re going to look at some signs and symptoms of
mental health conditions.
● Before we do, it’s important to understand that while you
might recognize some of these in yourself, that doesn’t
necessarily mean you have a diagnosable mental health
condition. If you relate to any of the conditions we discuss
today, I strongly encourage you to share that with your
parent/caregiver or another trusted adult.
● First, let’s watch a short video called “Ending the Silence.”
It goes over the ten most common signs of a mental health
condition, and it was created by the National Alliance on
Mental Illness—NAMI for short.
Show the video. Afterward, have the group discuss
these questions:
● How do you feel about what you just saw?
● Were you already aware of any of these signs of a
mental health condition? Were there any that were
new to you?
● How would you respond if you saw any of these signs
in a friend or family member?
● How can we make it easier to talk about
mental health?
Showing Up For Me and You Facilitator Guide | 13
Pass out the Symptoms of Mental Health Conditions
meeting aid.
SAY:
● It’s not always easy to tell the difference between expected
behaviors and signs of a mental health condition.
● But there are common symptoms of mental health
conditions that we can look out for, like the ones on the list
I just gave you.
Give the group a few minutes to review on their own.
Tell them they can ask questions if they want to clarify
anything. Here are a couple of questions that might come
up, with suggested responses you can provide:
● How do you make these symptoms better or make
them go away? (Treatment, such as therapy and
doctor-prescribed medications, can help. Behavioral
changes—like getting more sleep and exercise, and
meditating—are important, too. Alternative treatments
like acupuncture and meditation can also ease the
symptoms. First, though, it’s helpful to start talking
about the symptoms—being alone with the experience
can be really painful.)
● Is there one condition on the list that’s worse or better
than another? (No. That’s because every mental health
condition affects people differently. Some people can
be diagnosed with just one condition, and some can
have three or four simultaneously. Symptoms can be
more severe or less severe. In many cases, other people
may not even realize that someone has a mental health
condition.)
SAY:
● As I said earlier, you might recognize some of these
symptoms in yourself or others at times, but that doesn’t
necessarily mean you or they have a mental health
condition.
● Maybe you’ve experienced these symptoms for a short
time when going through a stressful or tough situation.
Anyone want to share an example of that?
Let the group share if they can. If needed, offer these
examples:
● You might get headaches or have trouble sleeping
before a big test, but those symptoms tend to go away
after the stressful event is over.
● If you go through a major life change, like switching
schools or moving away from your closest friends, you
might feel sad and lonely at rst. These symptoms can
get better as time passes and you settle in, make new
friends, and get used to a new routine.
SAY:
● On the other hand, symptoms of a mental health condition
affect a person’s thinking, feeling, behavior, or mood.
These conditions deeply impact day-to-day living and
may also affect the ability to relate to others.
● A mental health condition isn’t the result of one event.
Research suggests multiple, linking causes. Genetics,
environment, and lifestyle can inuence whether someone
develops a mental health condition. A stressful job or
home life makes some people more susceptible, as do
traumatic life events.
● If you ever experience anything like that, it’s important
that you share it with your parents or caregivers, or
another trusted adult in your life.
● Talking about our mental health means that we’re more
able to get the support we need. But sometimes we’re not
comfortable talking about it. We’ll focus more on that in
the next activity.
● Take the Symptoms of Mental Health Conditions
meeting aid with you as a reminder and share what you
learned with your friends and family.
Facilitation Script and Activity Guide

Showing Up For Me and You Facilitator Guide | 14
Facilitation Script and Activity Guide
Activity 2: Language Matters (15 minutes)
Materials:
● Your Language Matters meeting aid
(one for each participant)
● Recording devices, such as smartphones (optional)
● Pencils or pens
● Paper
Purpose: Participants nd out about mental health stigma,
learn how the language they use to talk about mental health
makes a difference, and create a video to help ght stigma.
Pass out the Your Language Matters meeting aid.
SAY:
● In this next part, we’re going to look at language and
really zero in on how we can remove the stigma, or shame,
that so often surrounds mental health issues. This stigma
is what can make it difcult and uncomfortable to even
have discussions about mental health.
● The handout I just gave you is one I hope you’ll take home
and refer to often. It gives examples of language to use
and language to lose when talking about mental health.
Give the group a minute to read the meeting aid.
● Is there any language on the handout that you’ve used
yourself or heard someone use? What was it?
● Using language that encourages understanding is key to
breaking down the stigma associated with mental health.
● Have you heard that word before, “stigma”? What does it
mean? (Give time to respond. If needed, say that stigma
is a negative attitude about a person, group, condition,
or circumstance that’s thought to be different or “less
than.”)
● Why do you think that mental health conditions have a
stigma related to them? (Give time to respond.)
● There’s also something called self-stigma. That’s the
shame a person feels about some part of themselves.
● Many people who live with a mental health condition
have, at some point, been blamed for it. They’ve been
called names. Their symptoms have been referred to as
“a phase” or something they could control “if they only
tried.” All of these are examples of stigma, and the person
can internalize these messages as true.
● So how can we ght stigma? What ideas do you have and
why would they help?
Let the group lead this conversation. If needed, offer
these ideas:
● Talk openly about mental health.
● Learn more about mental health.
● Show compassion for those who have a mental
health condition or who are struggling with a
mental health challenge.
● Be conscious of language. Gently let anyone you’re
talking to know when the language they’re using is
harmful. You could tell them something like, “When
you say [example], that can be harmful to people with
mental health conditions. It’s more helpful to say
[example].”
SAY:
● These were all great ideas. Now you’re going to work in
small groups to write or lm a short video message about
ghting mental health stigma. Use the ideas you just
discussed or come up with new ones.
Divide the group into small teams to write a script for or
lm a short video message (if smartphones are available).
When they’re done, have them share their messages with
the group. If they wrote a script, have them read it out loud
or act it out.
SAY:
● Your video messages are excellent. How could you share
your message with more people?
● Before we continue, let’s recharge with a stretch-and-
snack break.

Showing Up For Me and You Facilitator Guide | 15
Facilitation Script and Activity Guide
Stretch-and-Snack Break (10 minutes)
Materials:
● Nutritious snack items such as fresh fruit, trail mix,
granola bars, and water
● Paper plates or cups
● Disposable utensils
Purpose: During a stretch-and-snack break, participants
explore how movement and nutrition can affect the way
they feel.
Encourage everyone to choose their own stretch and do it
for one or two minutes. They can do this standing or sitting,
whatever feels good to them. If they’re unable to think of
one, show them a couple of your favorites.
SAY:
● How did stretching make your body feel? (Give time to
answer.)
● How does movement affect how you feel mentally?
(Give time to answer.)
● Did you know that what you eat can also affect how you
feel? Let’s get a snack and talk about that some more.
Have the group select whatever snacks they’d like. While
they eat, talk with them about how nutrition impacts
mental health.
SAY:
● We’re taking a snack break to give our brains some
energy.
● Foods have nutrients that can help you stay alert and
strong, and make you feel better.
● Do you notice a difference in how you feel when you’re
hungry compared to when you’ve had a nutritious meal or
snack? (Give time to answer.)
● What foods and drinks do you think keep your body and
mind strong? (Give time to answer.)
● Hope you’re all feeling recharged! Let’s move on to the next
activity, where we’ll get into self-care and what it means
to be resilient.
Activity 3: Building Resilience (15 minutes)
Materials:
● Paper (enough for everyone)
● Pencils or pens
● Large construction paper (enough for everyone)
● Small sticky notes
● Markers
● Getting the Right Start meeting aid
Purpose: Participants explore different types of self-care,
identify stressful and positive things in their lives, talk
about why it’s important to get help, and learn about taking
care of themselves.
SAY:
● Did you know that one out of every six people ages 6 to 17
experiences a mental health condition each year? What do
you think of that statistic? (Give time to respond.)
● When someone is struggling, what should they do? (Give
time to respond; if needed, offer “get help” as an answer.)
● Let’s nd out more about what it takes to get help if you or
someone you know is struggling with something.
Pass out the Getting the Right Start meeting aid. Use this
next discussion to help familiarize participants with the
points made in the handout and lead into a discussion about
self-care and coping.
SAY:
● Why do you think it’s important to tell someone about a
mental health challenge?
● What points on this handout do you nd most helpful?
Or surprising?
● Why do you think it’s important not to wait to get help?
● What do you do when you’re having a tough day? How
do you move forward when you’re struggling with
something, like a difcult assignment at school?
Showing Up For Me and You Facilitator Guide | 16
Facilitation Script and Activity Guide
● It’s okay to feel sad, hurt, or angry when you’re dealing
with a tough situation. Feeling our feelings—rather than
avoiding or trying to hide them—is a great way to process
them and take care of ourselves.
● One way to deal with tough situations is to practice
self-care. How do you dene that? What do you do for
self-care? (Give time to respond.)
● Your denitions are all great because self-care can mean
a lot of things.
● Taking a bath or writing in a journal are often our
go-to examples. But self-care can also mean:
• utilizing your support system
• giving yourself slack when you make a mistake or
fail at something
• saying no when something doesn’t feel good to you
• putting your phone down and taking a break from
connecting with others for a period of time
• advocating for yourself
• raising your voice to be heard
● Have you tried doing any of these? What was the situation
and how did it work out? (Give time to respond.)
● How do you think self-care is related to coping? (Give
time to respond. If you need to dene coping, it’s “the
things people do to help deal with stressful situations.”)
● What do you do to cope with tough situations? It may
be the same as what you do for self-care, or it may be
something different. (Give time to respond.)
● One example of a coping mechanism is to recognize the
things that stress you out and decide where or even if
they t into your life. That’s what you’re going to do now.
Ready?
Give everyone a piece of paper and have them make two
columns. In one column, they should list the things that
stress them out, such as a difcult relationship or an event
they’re not looking forward to. In the other column, they
should list the good stuff in their lives, such as a friendship
or an activity they love doing.
When they’re done with their lists, give everyone a piece of
construction paper and some sticky notes.
SAY:
● Draw a bubble in the middle of your paper.
● The inside of the bubble represents everything that feels
comfortable, enjoyable, and/or manageable for you. The
outside of the bubble represents everything that feels
uncomfortable, stressful, and/or difcult for you to manage.
● Write the items from your list on separate sticky notes—
one item per note.
● When you’re done, choose where to place each sticky note,
either inside or outside your bubble.
When everyone’s nished, give them the chance to share
and talk about their bubbles if they want. Whether they
share or not, everyone can discuss these questions:
● What are some ways you can open up a conversation
about a struggle you’re having? (If needed, offer these
ideas: Plan what you want to say; nd a private place
to talk; explain your challenge as clearly as you can;
come up with some next steps.)
● Why do you think it’s important to have these
conversations? (Answers could be: “So that it doesn’t
turn into a bigger issue down the line”; “The earlier you
speak up about something, the better chance you have
to manage the problem.”)
● What are the benets of being open or sharing with
someone when we’re struggling? (Answers could be:
“Having support makes it easier to deal with an issue”;
“You build a network of support—sharing with others
could make them more open to sharing with you when
they need help.”)
● Are you more likely to help someone else who is in
trouble than to help yourself? If so, why?
● Why did you make the placements you did?
● What do your placements say about what the items
mean to you or how you plan to deal with them in
your life?
SAY:
● Keep your bubble as a reminder of what you do and don’t
have room for in your life.
● Being aware of what things feel stressful and what you
can handle is one move toward taking care of yourself as
you navigate challenges. Remember you may not always
be able to avoid something that is causing stress.
● What does resilience mean to you? (Give time to answer;
if needed, share this denition: “Resilience is adapting
to or learning how to deal with life situations, such as
the ones you just identied. It’s a person’s ability to
bounce back after a setback, to learn from failure, and
to be willing to try again.”)
Showing Up For Me and You Facilitator Guide | 17
Facilitation Script and Activity Guide
● Resilience is something we can all build to help us through
day-to-day difculties. It’s also important to remember
that there are some things that, no matter how resilient
you are, may still get you down—big things like racism,
gender discrimination, or climate disasters. If we feel
overwhelmed by these challenges, that’s okay. And if
someone else feels hurt by them, it doesn’t mean they
aren’t being resilient enough.
● What do you think are some traits of resilient people?
(If needed, offer that resilient people are exible and
resourceful, set realistic expectations for themselves,
and are willing to learn from and seek solutions
to difcult or unexpected situations. Examples of
resilient people: an athlete who recovers from an injury
by doing physical therapy; a person who experiences
travel delays but nds another way to reach their
destination; a law school graduate who fails the bar
exam but keeps trying and passes the third time.)
● You’re going to go through difcult experiences in life.
Maybe you’ll make decisions that turn out poorly. The
point is, you’re learning and growing from all of it. Or,
at minimum, you’re just getting through it. This builds
your resilience.
● What traits of resilience do you think you have and what
ones do you want to develop?
● Remember, being resilient doesn’t mean handling
everything alone. How is asking for support part of being
resilient?
● Why do you think failure can sometimes be okay?
● How do you think setting boundaries plays a role in being
resilient? (If needed, offer: “Boundaries are limits
people create to protect themselves from being hurt,
manipulated, taking on too much, or being taken
advantage of. A boundary looks like saying no to a
request from a friend, not checking email late at night,
or speaking up when a situation feels off.”)
● Setting boundaries isn’t always easy. It takes practice
to communicate how you feel. Have you ever had to
set boundaries with a friend or in a situation where
you weren’t comfortable? How did you do it? What, if
anything, would you have done differently?
Stretch Break (5 minutes)
Purpose: Give the group a short stretch/bio break.

Showing Up For Me and You Facilitator Guide | 18
Facilitation Script and Activity Guide
Activity 4: Supporting Others (15 minutes)
Materials:
● How to Help a Friend meeting aid
(one for each participant)
● Active Listening Checklist meeting aid
(one for each participant)
● Pencils or pens
● Paper
Purpose: Participants learn how to support a friend
or family member who’s struggling and practice active
listening.
SAY:
● Knowing how to use your voice and seek help is important
for your self-care and mental health. What would you
do if you shared your problem with someone who wasn’t
supportive or wasn’t able to help you? (Let the group
know this is a way to practice resilience: they can
nd support or seek advice from other resources or
identify others who might be able to help them. If they
need help with ideas, tell them they could try to nd
someone else in their family or community, look for
resources from a school counselor or faith leader, or
nd support in a crisis text line or hotline.)
● Knowing how to get help for yourself can also give you
skills to support a friend who is struggling.
● When you spend your time and energy helping someone
else, it can have a positive impact on your own self-
esteem.
● Maybe you can do something like that for a friend, too.
Have you ever had regular check-ins with friends just to
ask how they’re doing?
● Can you always tell when someone’s struggling with
something? (Give time to respond.)
● Probably not. If we open up and share how we are doing,
they might be more willing to share with us.
● It’s also important to know your limits and be realistic
about what support you can offer.
● You can be there for friends and family, but you might not
be able to help with a serious mental health condition.
What would you do if you were concerned with your
friend’s health or safety? (If needed, say: “Seek help
from a trusted adult or a trained professional.”)
Pass out the How to Help a Friend meeting aid. Tell the
group it gives tips on how to start the conversation, offer
support, and be a friend. Have the group take turns reading
each section out loud. Ask if anything they read feels
familiar or if they’ve experienced it themselves.
SAY:
● One important way to help a friend is by actively listening
to them.
● What does it mean to be an active listener? (Give time to
respond. If needed, say: “It means to focus on not only
the words someone is saying but also what’s being
communicated. It also means to reect and respond
thoughtfully.”)
● Do you know someone who is a good listener? What makes
them that for you? (Give time to respond.)
● As you’ve just pointed out, there are some skills to being
an active listener and you’ll practice them today.
Give everyone the Active Listening Checklist meeting aid
and have them read through the do’s and don’ts of being an
active listener.
Give each participant a pen and paper.
SAY:
● Write down a general issue you or someone you know is
dealing with on a piece of paper. It could be something like
stress about the future, a ght with a sibling, something
you read on social media, or a situation where you felt
left out. You don’t need to sign your paper—everyone will
remain anonymous.
● Hand me your paper when you’re done.
Fold the papers and place them in a bowl. (Read them
beforehand to make sure they’re general enough and will
work for this activity.)
Divide the group into teams of three. One team member will
be the Sharer, one will be the Listener, and one will be the
Observer. If you can’t form enough teams of three:
● For a two-person team, you or another facilitator/
volunteer can be the Observer.
● For a four-person team, two people can be Observers.
SAY:
● One of you will be the Sharer. You’ll share a tough
experience picked from a paper in the bowl.

Showing Up For Me and You Facilitator Guide | 19
Facilitation Script and Activity Guide
● One of you will be the Listener. You’ll listen to the Sharer,
using techniques from the Active Listening Checklist.
Take a moment to review it again now if you’d like, before
your teammate starts sharing with you.
● And one of you will be the Observer. As the Sharer and
Listener do their thing, you’ll use the checklist to check
off the active listening traits that you see or hear. You can
also make notes on the checklist.
● Before you start, take a minute to decide which role each
of you wants to play.
Give the group ve to ten minutes for this activity. Give a
warning when there’s a minute left so they can wrap up.
Then get the group back together to discuss what they did
in their teams.
SAY:
● Sharers, what did you notice about the Listener? What
skills did they use that showed you they were actively
listening?
● Listeners, what were you able to pick up on from the
Sharer when you really listened to them?
● Observers, what active listening traits did you notice
most strongly? Are there any you didn’t check off? How
might they have helped in this situation?
● How do you all think active listening helped the person
who was sharing their problem? Did it help them nd a
solution or feel better?
● What do you think are the most important traits of active
listening?
● Do you think you need to have an answer to someone’s
problem to be supportive of them? (Answers could be:
“Sometimes just listening and caring is enough”; “It’s
important to let another person express themselves.”)
Note to facilitator: If the group wants to continue
practicing active listening, you can incorporate this activity
into a future troop meeting as time allows.
Reection and Wrap-up (5–10 minutes)
Materials:
● Suggestion box
● Pencils or pens
● Paper
Purpose: Participants reect on their impressions of
mental health when they arrive. They think about ways to
support their mental wellness.
Give the group time to respond to these reection questions:
● Look back at how you described mental health. Did
anything change? If so, what?
● What is something new you learned about mental
health and mental wellness?
● We covered a lot of topics today. What activity or
discussion did you nd most helpful or useful? Why?
● What immediate changes will you make to support
your own mental health and help others? (Answers
might be: “Talk to a trusted adult”; “Practice self-care”;
“Be more aware of my friend’s emotions”; or “Know
when and how to seek help if I need it.”)
SAY:
● Before you go, let’s do a quick, calming breathing exercise.
Mindful breathing is something you can do anytime,
anywhere to calm yourself or a friend, or to cope with a
stressful situation. Let’s do one type of mindful breathing
called a “box breath.”
Have participants:
1. Inhale through their noses for four seconds
2. Hold their breath for four seconds
3. Exhale slowly through their mouth for four seconds
4. Pause quietly for four seconds
Do this for a few rounds.
(Tip: You can trace the shape of a box in the air with your
nger while you count, to help visualize the four steps of
the breath.)
SAY:
● Do you think you’ll try mindful breathing the next time
you feel worried or stressed? It’s a great self-care practice!
● I am so glad you joined me today. Thank you for sharing
and being respectful!
Before the group leaves, let them know what the suggestion
box is and how to use it. Have them put anonymous
feedback, questions, or comments into the box.

Showing Up For Me and You Facilitator Guide | 20
We recommend the following additional steps to keep lines of communication open with parents/caregivers and to continue
integrating mental wellness into Girl Scout activities:
● Send a follow-up email to parents and caregivers. Share what their Seniors and Ambassadors did and learned about
mental wellness. See the Customizable Post-Event Email to Parents/Caregivers (p. 22).
● Send a follow-up email to your council to let them know how your Showing Up For Me and You Patch Program went. If
your council has prepared a survey for you to ll out, send that in.
● Incorporate mental wellness moments in future troop meetings. Check out GSUSA’s Resilient. Ready. Strong. patch program
for some ideas, such as playing music or creating a “happy box” with things that make Seniors and Ambassadors
smile. You can also ask them to choose or vote on what kind of wellness activities they’d like to do to start or end each
meeting. It might be a breathing exercise, a yoga move, or a moment of silence to think about what they’re grateful for.
● For Seniors and Ambassadors who are college bound or thinking about college, suggest that they take a look at the
NAMI guide Starting the Conversation: College and Your Mental Health, written for both students and parents/
caregivers. College can be emotionally challenging, and they can prioritize their mental health by looking for on-
campus support, social connections, and ways to connect with their new community before they start.
Next Steps

Showing Up For Me and You Facilitator Guide | 21
Customizable Invitation Email to Parents/Caregivers
Next Steps
Use this email template to help you reach out to Seniors and Ambassadors and their families or caregivers in
advance of conducting the Showing Up For Me and You patch program. This is the suggested language for inviting
participants. Customize as needed.
Dear Girl Scout Families and Caregivers,
Seniors and Ambassadors are invited to take part in a 90-minute Mental Wellness Patch Program called Showing Up For
Me and You on [DATE]. Girl Scouts of the USA collaborated with experts at the National Alliance on Mental Illness (NAMI) to
develop the program, and also received input from other mental health professionals and Girl Scout council leaders. It has
been generously funded by the HCA Healthcare Foundation.
Girl Scouts will participate in activities and have discussions about ghting mental health stigma, dealing with stressful
situations, building resilience in the face of challenges, and supporting friends who are struggling. This will be a supportive
space to learn about mental wellness.
[Note to facilitator: If your meeting is in a location different from your regular troop meetings, provide the address and
directions.]
If you have any questions, please contact me or the council directly. I look forward to seeing your Girl Scout on [DATE].
Thank you for supporting Girl Scouts.
Best regards,
[YOUR NAME]

Showing Up For Me and You Facilitator Guide | 22
Customizable Post-Event Email to Parents/Caregivers
Next Steps
Use this email template to help you send a follow-up email to parents and caregivers. Share what their Seniors and
Ambassadors did and learned about mental wellness. This is suggested language for a post-event communication
to parents and caregivers. Customize as needed.
Dear Girl Scout Families and Caregivers,
Today, your Girl Scouts participated in the Mental Wellness Patch Program for Seniors and Ambassadors: Showing Up For
Me and You. They came up with strategies to ght mental health stigma, learned how to cope with tough situations in their
lives, and practiced active listening to support friends who are struggling.
[Note to facilitator: Include any additional information you’d like about how the program went, the positive outcomes you
observed, and/or your plans to incorporate mental wellness moments into future meetings.]
If you have any questions, please contact me or the council directly. Thank you for supporting Girl Scouts.
Best regards,
[YOUR NAME]

© 2023 Girl Scouts of the United States of America (GSUSA). All rights reserved. Not for commercial use. This material
is proprietary to GSUSA and may be used, reproduced, and distributed exclusively by GSUSA staff, councils, Girl Scout
volunteers, service units, and/or troops solely in connection with Girl Scouting.
Showing Up For Me and You Facilitator Guide | 23
Meeting Aids
Use these meeting aids to facilitate this program.
For Facilitators:
● For Facilitators: Mental Health Terms to Know
● For Facilitators: Symptoms of Mental Health Conditions
● For Facilitators: What to Know About Identity, Culture, and Mental Health
● For Facilitators: Girl Scout Safety Activity Checkpoints—Overall Health, Well-Being, and Inclusivity
For Seniors and Ambassadors:
● For Seniors and Ambassadors: Symptoms of Mental Health Conditions
● For Seniors and Ambassadors: Your Language Matters
● For Seniors and Ambassadors: Getting the Right Start
● For Seniors and Ambassadors: How to Help a Friend
● For Seniors and Ambassadors: Active Listening Checklist

Anxiety Disorders: A group of related conditions, each having unique symptoms. However, all anxiety
disorders have one thing in common: persistent, excessive fear or worry in situations that are not
threatening. Everyone can experience anxiety, but when symptoms are overwhelming and constant—often
impacting daily living—it may be an anxiety disorder.
Attention Decit Hyperactivity Disorder (ADHD): A developmental disorder dened by inattention
(trouble staying on task, listening), disorganization (losing materials), and/or hyperactivity-impulsivity
(dgeting, difculty staying seated or waiting). While ADHD occurs among people of all identities, it is
generally underdiagnosed in girls.
Bipolar Disorder: Causes dramatic shifts in a person’s mood, energy, and ability to think clearly.
Individuals with this disorder experience extreme high and low moods, known as mania and depression.
Some people can be symptom-free for many years between episodes.
Borderline Personality Disorder (BPD): A condition characterized by difculties regulating emotion.
This means that people who experience BPD feel emotions intensely and for extended periods of time;
it’s harder for them to return to a stable baseline after an emotionally triggering event. This difculty can
lead to impulsivity, poor self-image, stormy relationships, and intense emotional responses to stressors.
Struggling with self-regulation can also result in dangerous behaviors such as self-harm (e.g., cutting).
Clinical Social Workers: Practitioners trained to evaluate a person’s mental health and use therapeutic
techniques based on specic training programs. They’re also trained in case management and
advocacy services.
Counselors, Clinicians, Therapists: Masters-level healthcare professionals trained to evaluate a person’s
mental health and use therapeutic techniques based on specic training programs. They operate under a
variety of job titles—including counselor, clinician, therapist, or something else—based on the
treatment setting.
Depression: Involves recurrent periods of clear-cut changes in mood, thought processes, and motivation
lasting for a minimum of two weeks. Changes in thought processes typically include negative thoughts and
hopelessness. Depression can also affect sleep/energy, appetite, and weight.
Eating Disorders: A group of related conditions involving a preoccupation with food and body weight
that cause serious emotional and physical problems. Each condition involves extreme food and weight
issues; however, each has unique symptoms that separate it from the others. Common eating disorders are
anorexia nervosa, bulimia nervosa, and binge eating disorder.
Mental Health Terms To Know
Conversations about mental health and mental wellness are central to the Girl Scout Junior Knowing My
Emotions, Cadette Finding My Voice, and Senior & Ambassador Showing Up For Me and You patch programs.
Before leading any discussion on mental health and mental wellness, familiarize yourself with these
denitions of mental health terms that may come up. Doing so will help you to lead a lively, productive, and
informed conversation among troop members. This glossary from the experts at the National Alliance on
Mental Illness (NAMI) provides denitions for mental health terms that may come up.
This glossary from the experts at the National Alliance on Mental Illness provides denitions for mental
health terms that may come up.
24
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
Mental Health Terms to Know

Mental Illness: A condition that affects a person’s thinking, feeling, or mood. These conditions may affect
someone’s ability to relate to others and function day to day. Each person will have different experiences,
even people with the same diagnosis.
Obsessive Compulsive Disorder (OCD): Characterized by repetitive, unwanted, intrusive thoughts
(obsessions) and irrational, excessive urges to do certain actions (compulsions). Although people with
OCD may know that their thoughts and behavior don’t make sense, they are often unable to stop them.
Symptoms typically begin during childhood, the teenage years, or young adulthood.
Post-Traumatic Stress Disorder (PTSD): Traumatic events—such as an accident, assault, military
combat, or a natural disaster—can have lasting effects on a person’s mental health. PTSD can occur at any
age. Symptoms, which include reexperiencing, avoidance, and arousal, usually begin within three months
after experiencing or being exposed to a traumatic event. Symptoms of depression, anxiety, or substance
use often accompany PTSD.
Psychiatrists: Licensed medical doctors who have completed psychiatric training. They can diagnose
mental health conditions, prescribe and monitor medications, and provide therapy. Some have completed
additional training in child and adolescent mental health, substance use disorders, or geriatric psychiatry.
Psychologists: Practitioners who hold a doctoral degree in clinical psychology or another specialty such
as counseling or education. They are trained to evaluate a person’s mental health using clinical interviews,
psychological evaluations, and testing. They can make diagnoses and provide individual and group
therapy.
Self-harm: Also called self-injury, this is when a person hurts themselves on purpose. One common
method is cutting the skin with a sharp object, but anytime someone deliberately hurts themselves, it is
classied as self-harm. Some people feel an impulse to cause burns, pull out hair, or pick at wounds to
prevent healing. Extreme injuries can result in broken bones.
25
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
Mental Health Terms to Know

26
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
It’s important for adult leaders of Girl Scouts to know and understand the symptoms of mental health conditions;
however, noticing any of these symptoms in yourself or someone else doesn’t necessarily mean a diagnosable
mental health condition is present. Refer to the meeting aid “Girl Scout Safety Activity Checkpoints—Overall
Health, Well-Being, and Inclusivity” for further guidance on addressing and reporting mental health concerns
about a Girl Scout.
Symptoms of Mental
Health Conditions
Conversations about mental health and mental wellness are central to the Girl Scout Junior Knowing My
Emotions, Cadette Finding My Voice, and Senior & Ambassador Showing Up For Me and You patch programs.
Before leading any discussion on mental health and mental wellness, familiarize yourself with the signs and
symptoms of mental health conditions. Doing so will help you to lead a lively and productive conversation
among troop members. This tip sheet explains ve of the most common mental health conditions that may
come up in your discussions with troop members.
Anxiety:
Gets upset when not on time for things like homeroom, practices, and parties; needs the comfort
of a schedule and reacts negatively when plans change; seeks perfection in grades, extracurriculars,
or cleanliness.
Attention Decit Hyperactivity Disorder (ADHD):
Has difculty paying attention and listening when spoken to; is hyper focused on things they enjoy; moves
constantly; talks excessively and over people; jumps from subject to subject; loses things a lot; starts many
tasks but has a hard time nishing them; is forgetful; has sensory sensitivities.
Depression:
Stops participating in things they used to enjoy; is not responsive to texts and invites; is easily frustrated,
irritated, or short-tempered; could also be overachieving or taking on too much.
Eating Disorders:
Eats too little or too much; has an intense fear of gaining weight; engages in excessive exercise;
worries over calorie intake.
Post-Traumatic Stress Disorder (PTSD):
Avoids situations that make them recall the traumatic event; experiences nightmares or ashbacks about
the trauma; plays in a way that repeats or recalls the trauma; acts impulsively or aggressively; frequently
feels nervous or anxious; experiences emotional numbness; has trouble focusing at school
Symptoms of Mental Health Conditions

27
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
What to Know About Identity, Culture, and Mental
What to Know About Identity,
Culture, and Mental Health
Girl Scouts have a range of identities and come from a range of cultures. The following information, adapted
from the experts at the National Alliance on Mental Illness (NAMI), will help you understand how identity and
cultural background can affect someone’s responses to mental health issues and access to treatment. Each
of the communities below consists of sub-communities with diverse cultures and identities. It’s important to
recognize and respect the uniqueness of each. Mental health needs and experiences vary among subgroups.
Asian American and Pacic Islander (AAPI) Community
This racial identity is inclusive of 50 distinct ethnic groups speaking more than 100 languages, with
connections to Chinese, Indian, Japanese, Filipino, Vietnamese, Korean, Hawaiian, and other Asian and
Pacific Islander ancestries.
It’s a common cultural experience for members of the AAPI community to experience a deep sense of
community and strong family bonds, which can help them build resilience to deal with challenges.
Many second-generation members of the AAPI community struggle to nd balance between traditional
cultural values and the pressure to assimilate into the norms of mainstream (white) American society.
Barriers to addressing mental health issues include:
•
Language, especially when seeking counseling for sensitive or personal issues.
•
Fear of jeopardizing immigration status or citizenship.
•
Stigma and shame (don’t want others to have a negative opinion of them).
•
The “model minority” myth: a misleading belief that Asian Americans and Pacic Islanders are
uniformly well adjusted, hard-working, and well educated, and enjoy more socioeconomic success
than other people of color. This stereotype can result in others not attending to challenges expressed
by members of the AAPI community.

28
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
What to Know About Identity, Culture, and Mental
Black/African American Community
This racial identity is inclusive of ethnic groups who can trace their origins in total or in part to the continent
of Africa. The experience of being Black in America varies widely, but shared cultural factors play a role in
mental health.
Experiencing racism, discrimination, and inequity can signicantly affect a person’s mental health.
Being treated or perceived as “less than” because of skin color can be stressful and even traumatizing.
Black adults in the U.S. are more likely than white adults to report persistent symptoms of emotional
distress, such as sadness, hopelessness, and feeling like everything is an effort.
Barriers to addressing mental health issues include:
•
Inhibited geographic access to quality mental health care due to racial segregation and
inequitable distribution of resources.
•
Socioeconomic factors that limit access to treatment options.
•
Internalized stigma: the perception, especially among older Black adults, of mental health conditions
as personal weaknesses.
•
Mistrust of healthcare providers due to bias and lack of cultural understanding.
•
Preference to seek support from faith communities.
Hispanic / Latinx Community
In the U.S., this community includes people from many different nations and regions of the world: Mexico,
Puerto Rico, Cuba, Central America, and South America, among others. While largely regarded as one
community, it’s comprised of various racial and ethnic groups.
Hispanic/Latinx communities are just as vulnerable to mental illness as other racial and ethnic groups,
but, due to structural and institutional barriers, they don’t have equal access to quality treatment. More
than half of Hispanic/Latinx people aged 18–25 with serious mental illness may not receive treatment.
Barriers to addressing mental health issues include:
•
Language, especially when seeking counseling for sensitive or personal issues.
•
Lack of health insurance coverage.
•
Socioeconomic factors and cost of healthcare services.
•
Fear of jeopardizing immigration status or citizenship.
•
Mistrust of healthcare providers due to bias and lack of cultural understanding.
•
Stigma and shame: This community fears being labeled “crazy” and doesn’t want to bring
shame to their family. They prefer to keep challenges at home private.

29
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
What to Know About Identity, Culture, and Mental
Indigenous / Native Community
Indigenous/Native people are those who have been living on this land prior to European colonization. There are 574
federally recognized tribal nations in the U.S., as well as tribes living without official recognition. These nations include
over 200 Indigenous languages (and many dialects within those languages) and countless diverse cultures, traditions,
and histories.
The traumatic history of extermination, displacement, and forced assimilation of Indigenous/Native peoples
continues through economic and political marginalization, discrimination, and inadequate access
to education, healthcare, and social services.
The multigenerational trauma that Indigenous/Native people have endured can lead to mental illness,
substance use disorders, and suicide.
Suicide rates for Indigenous/Native adolescents are more than double the rate for White adolescents.
Barriers to addressing mental health issues include:
•
Language, especially when seeking counseling for sensitive or personal issues.
•
Indian Health Services (IHS) is underfunded and unable to offer services to meet mental health
needs of the community.
•
Community members tend to live in rural and isolated locations with high rates of poverty
and unemployment.
•
Programs don’t often provide treatment that is culturally, spiritually, and traditionally appropriate.
LGBTQIA+ Community
The Lesbian, Gay, Bisexual, Transgender, Queer or Questioning, Intersex, and Asexual (LGBTQIA+) community
represents a diverse range of identities and expressions of gender and sexual orientation. (The “+” represents
all other non-cisgender gender identities and non-heterosexual sexual orientations that are not captured by the
letters.) Members are also diverse in race, religion, ethnicity, nationality, ability, and socioeconomic class. It’s
important to consider the combined and overlapping aspects of a person’s identity.
Many in the LGBTQIA+ community face discrimination, prejudice, denial of civil and human rights,
harassment, and family rejection, which can lead to new or worsened symptoms of a mental
health condition.
LGBTQIA+ adults are more than twice as likely as heterosexual adults to experience a mental health
condition. Transgender individuals are nearly four times as likely as cisgender individuals (people
whose gender identity corresponds with the gender assigned to them at birth) to experience one.
Substance use and abuse is high among LGBTQIA+ individuals, and they have a 120% higher risk of
experiencing homelessness due to family rejection and discrimination.
Barriers to addressing mental health issues include:
•
Discrimination and bias within the healthcare system.
•
The outdated notion that questioning one’s gender identity is a mental health condition.
•
Mental health care providers often lump the entire LGBTQIA+ community together instead of
addressing each sub-community’s unique challenges, experiences, and rates of mental illness.

30
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
What to Know About Identity, Culture, and Mental
People with Disabilities
Nearly one in five (61 million) people in the U.S. are living with a disability. Disabilities can be physical or
mobility-related, cognitive, developmental, intellectual, or sensory. A disability is generally defined as such
when an impairment substantially limits at least one major life activity. Disabilities can be visible or not; it
should never be assumed whether or not someone has one.
Though discrimination against people with disabilities is against the law, they often continue to face
discrimination and unequal access in employment, housing, medical care, and insurance coverage.
Many people with disabilities experience physical challenges, including immobility or extreme pain,
and social challenges, such as isolation or being excluded from invitations to social events and
recreational activities.
Given the stigma, lack of understanding about disabilities, and the need to navigate a society that is built
for people without disabilities, many people with disabilities try to hide or mask their disability. This is
burdensome and emotionally taxing.
Barriers to addressing mental health issues include:
•
A perception that people with disabilities need to be “xed,” cannot function fully in society,
or have a “defect”.
•
A perception that mental health symptoms are to be expected given a person’s circumstances,
and that they are unlikely to benet from care.
•
Lack of integrated care; physicians treat people’s physical issues but often view any mental health
symptoms as a by-product of the physical experience.
•
Difculty communicating, either verbally or physically.
•
Poverty and lack of access to care due to employment discrimination; this population is three times as
likely as people without disabilities to live in poverty.

31
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
Activity Checkpoints for Overall Health, Well-Being, and Inclusivity
Activity Checkpoints for Overall Health,
Well-Being, and Inclusivity
Presenting the Girl Scout Junior Knowing My Emotions, Cadette Finding My Voice, and Senior & Ambassador
Showing Up For Me and You patch programs will expand your knowledge of mental health and wellness
issues. It may also lead to revealing conversations with your Girl Scouts. You may become aware of
concerning signs and symptoms among your troop. This excerpted section of the Safety Activity Checkpoints
contains guidance for addressing and reporting mental health concerns about a Girl Scout. Contact your
council with questions or to obtain the full version of the Safety Activity Checkpoints.
Girl Scout councils require an annual health history form to be completed and signed by one parent/guardian for
every Girl Scout and kept on file with the troop leader.
Follow council guidelines to comply with this requirement. The form should reflect any significant medical
conditions, health issues, or allergies, and be updated each year. The form can also reflect any over-the-counter
medications that a Girl Scout is not permitted to take, if there are any.
If parents or caregivers send medication on trips or activities, it should be in its original labeled container and
controlled and administered by one designated adult. Health history forms can be shared with the site, camp
physician, or nurse ahead of time.
Always keep a current and signed health history form for each Girl Scout member with you when traveling.
Your council may require an updated midyear health history form for overnight trips. For physically demanding
activities, such as water sports, horseback riding, or skiing, an additional current health history form may be
obtained to make sure all adults are aware of any current medical conditions or special needs. Councils will retain
all health history forms in accordance with state record retention requirements and laws.
Health History Form
Some councils also require a health exam for any activity that is three overnights or longer, which may include
resident camp. Again, follow your council’s guidelines with respect to health exams. In most cases, the health
exam needs to have been completed within one year of the last date of the trip in order for Girl Scout members to
participate. Your council may require a current health exam for adult volunteers who participate in trips of three
nights or more as well; be sure to ask your council about their health exam policy. A health exam can be given by
a licensed physician, a nurse practitioner, a physician’s assistant, or a registered nurse. The medical provider must
sign the health exam form.
For large events or trips longer in duration, such as resident camp or a weeklong trip to a ranch, the designated
health professional at the trip location is responsible for collecting all health exam forms and health history forms
for members and adults.
Health exam forms and health history forms are to be shared only with designated health professionals and council
staff responsible for coordinating them. All health and medical information are private (by law) and must not be
shared or publicly available, so keep forms safe and secure. Only share information on a need-to-know basis.
Councils will retain all health exam forms in accordance with individual state record retention requirements
and laws.
Health Exams and Health Exam Forms
32
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
Activity Checkpoints for Overall Health, Well-Being, and Inclusivity
Issues or questions with respect to vaccination exemption periodically arise with activity and trip participation.
Vaccine exemption laws vary by state and focus on public and private school attendance more directly than they do
for youth organizations. Therefore, it is best to obtain local and state legal guidance and proceed in accordance with
the state law as it applies to school attendance. A general overview of state laws regarding school immunization
exemption is provided and annually updated on the National Conference of State Legislatures website.
If you have any questions about your obligation to communicate a Girl Scout member’s non-immunization with
other troop parents or caregivers, contact your Girl Scout council for legal guidance as privacy laws may apply.
Absent state laws that speak directly to vaccines and communicating non-immunization with parents of youth
groups, the guidance is to follow the standard and protocol as it pertains to school attendance.
For information on COVID-19 vaccination, see Coronavirus Safety in Girl Scouts.
Vaccination and Immunization
Mosquitoes, ticks, and insect bites are an inherent risk to any warm weather outdoor activity. Ensure parents and
guardians are aware of the need to have their children properly covered, preferably with closed shoes and light-
colored clothing and socks. It is important to advise parents, guardians, and Girl Scout members of this risk and the
safety precautions they should take. The understanding that your troop or council cannot be held responsible for
tick bites can be reinforced with a waiver reference on a permission slip.
An excellent source for learning more is the Tick and Lyme disease prevention section of UptoDate.
To learn more about using insect repellent safely, visit the Environmental Protection Agency website at Repellents:
Protection against Mosquitoes, Ticks, and Other Arthropods. To learn more about safely using DEET directly
on the skin and on children, check out EPA DEET.
Mosquitoes, Ticks, and Lyme’s Disease Prevention
Adults are responsible for making Girl Scouts a place where members are as safe emotionally as they are physically.
Protect their emotional safety by creating a team agreement and coaching Girl Scouts to honor this agreement.
Team agreements typically encourage behaviors like respecting diverse opinions and feelings, resolving conflicts
constructively, avoiding physical and verbal bullying or clique behavior, practicing fairness, and showing positive,
respectful, and helpful communication with others.
Emotional Safety
Physical, verbal, emotional, or sexual abuse of Girl Scouts is forbidden. Sexual pressure, sexual advances, improper
touching, sexual communication such as text messaging, and sexual activity of any kind with Girl Scout members is
not tolerated. If you witness or experience any behavior of this nature, notify appropriate council staff immediately.
Incidences of abuse of any kind will result in immediate council intervention. Volunteers are responsible for
following their council’s guidelines for reporting any direct information or concern around physical, verbal,
emotional, or sexual abuse with respect to girls.
Physical or Sexual Abuse
33
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
Activity Checkpoints for Overall Health, Well-Being, and Inclusivity
Youth violence or bullying is also not tolerated in Girl Scouts. Youth violence occurs when young people intentionally
use physical force or power to threaten or harm others. Bullying is a form of youth violence. Volunteers should
become familiar with the signs, risk factors, and preventive measures against this type of behavior. If you witness
or experience any behavior of this nature, notify the appropriate council staff for guidance. The CDC provides
excellent resources on this topic, including:
CDC Youth Violence
CDC Fast Fact: Preventing Bullying
CDC Youth Violence Prevention Strategies
Youth Violence and Bullying
All states, the District of Columbia, American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, and the
U.S. Virgin Islands have specific laws which identify persons who are required to report suspected child abuse to
an appropriate agency. Therefore, if you witness or suspect child abuse or neglect, whether inside or outside of Girl
Scouting, always notify the appropriate council staff immediately and follow your council’s guidelines for reporting
your concerns to the proper agency within your state. For more information, please review these available resources:
U.S. Department of Health & Human Services; Child Abuse and Neglect
U.S. Department of Health & Human Services: How to Report Child Abuse and Neglect
Child Welfare Information Gateway: Mandatory Reporters of Child Abuse and Neglect
CDC: Child Abuse and Neglect Prevention
Child Abuse
As an adult volunteer overseeing the activities and behaviors of young people, you may witness signs of self-harm
or the desire to harm others. Self-harm can be expressed physically through activities such as cutting, burning,
bruising, excessive scratching, hair pulling, poisoning, or drug use. Another form of self-harm is suicidal ideation,
which can be expressed verbally or with the written word. Yet another harmful expression involves harm to others,
which can be expressed verbally or with physical aggression. If a situation of this nature is observed or comes to
your attention in any form, always notify an appropriate council staff member immediately and follow your council
guidelines with respect to next steps. The CDC provides informative guidance around identifying and responding to
harmful behaviors: Self-Directed Violence and Other Forms of Self-Injury and also a section on at-risk youth:
Help Youth At Risk for Adverse Childhood Experiences (ACEs).
Mental Health and Safety
34
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
Activity Checkpoints for Overall Health, Well-Being, and Inclusivity
Girl Scouts is committed to making reasonable accommodations for the inclusion of physical and cognitive
disabilities. Talk to Girl Scout members of all abilities and their caregivers. Prior to an activity, always ask about
needs and accommodations. Always be sure to contact the location, facility, and/or instructors to ensure they are
able to accommodate those with disabilities. For more information visit Disabled World. Whenever possible, the
individual Safety Activity Checkpoints will provide additional resources specific to that sport or activity. Be sure to
reference these resources when planning to include a Girl Scout member with a disability. Our goal is to include all
girls with a desire to participate.
Include Girl Scout Members with Disabilities
In addition to physical and social-emotional disabilities, consider the history, culture, and past experiences of
the Girl Scout members in your troop that could affect their ability to equally participate in an activity. Work
with members and families to understand how an activity is perceived or experienced. Ensure that all Girl Scout
members and their families feel comfortable and have access to whatever is needed to fully participate, such as
proper equipment, prior experiences, and the skills needed to enjoy the activity.
Equity

35
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation
© 2023 Girl Scouts of the United States of America. All rights reserved.
Adult Facilitators | Knowing My Emotions, Finding My Voice,
Showing Up For Me and You
It’s important for adult leaders of Girl Scouts to know and understand the symptoms of mental health conditions;
however, noticing any of these symptoms in yourself or someone else doesn’t necessarily mean a diagnosable
mental health condition is present. Refer to the meeting aid “Girl Scout Safety Activity Checkpoints—Overall
Health, Well-Being, and Inclusivity” for further guidance on addressing and reporting mental health concerns
about a Girl Scout.
Symptoms of Mental
Health Conditions
Conversations about mental health and mental wellness are central to the Girl Scout Junior Knowing My
Emotions, Cadette Finding My Voice, and Senior & Ambassador Showing Up For Me and You patch programs.
Before leading any discussion on mental health and mental wellness, familiarize yourself with the signs and
symptoms of mental health conditions. Doing so will help you to lead a lively and productive conversation
among troop members. This tip sheet explains ve of the most common mental health conditions that may
come up in your discussions with troop members.
Anxiety:
Gets upset when not on time for things like homeroom, practices, and parties; needs the comfort
of a schedule and reacts negatively when plans change; seeks perfection in grades, extracurriculars,
or cleanliness.
Attention Decit Hyperactivity Disorder (ADHD):
Has difculty paying attention and listening when spoken to; is hyper focused on things they enjoy; moves
constantly; talks excessively and over people; jumps from subject to subject; loses things a lot; starts many
tasks but has a hard time nishing them; is forgetful; has sensory sensitivities.
Depression:
Stops participating in things they used to enjoy; is not responsive to texts and invites; is easily frustrated,
irritated, or short-tempered; could also be overachieving or taking on too much.
Eating Disorders:
Eats too little or too much; has an intense fear of gaining weight; engages in excessive exercise;
worries over calorie intake.
Post-Traumatic Stress Disorder (PTSD):
Avoids situations that make them recall the traumatic event; experiences nightmares or ashbacks about
the trauma; plays in a way that repeats or recalls the trauma; acts impulsively or aggressively; frequently
feels nervous or anxious; experiences emotional numbness; has trouble focusing at school
Symptoms of Mental Health Conditions
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation.
© 2023 Girl Scouts of the United States of America. All rights reserved.
36
Cadettes (Grades 6-8) | Finding My Voice
Senior and Ambassador (Grades 9-12) | Showing Up For Me and You
■
Mental health condition
■
The weather is unpredictable
■
My daughter has
schizophrenia
■
Person with a mental
health condition
■
Lives with, has or experiences
The words you use matter. You can break down
negative stereotypes and give people hope by
choosing words that are more relatable and
promote understanding. This simple but caring
approach may help people feel more comfortable
and willing to talk openly about mental health
and to reach out for support early.
Tips for Talking
About Mental Health
Tips for Talking
About Suicide
When talking about suicide, consider other
meanings your words may have. For example,
“committed suicide” implies that suicide is a crime.
You can help eliminate the misunderstanding
and stigma that pre vent people from speaking up
and getting support by choosing words that are
clearer and more neutral.
Matters
Language
■ Brain disorder or brain
disease
■ The weather is bipolar
■ My daughter is schizophrenic
■ Consumer, client or patient
■ Su ers from, a icted with or
mentally ill
INSTEAD OF
CONSIDER
SAYING
CONSIDER
SAYING
■ Suicide attempt/
attempted suicide
■ Died by suicide/
suicide death
■ Took their own life
■ Died as the result of
self-infl icted injury
■ Disclosed
■ Failed suicide or
unsuccessful attempt
■ Successful or completed
suicide
■ Committed suicide
■ Chose to kill him/herself
■ Threatened
INSTEAD OF
Language
Your
Your Language Matters
Supports Activity 2 for Finding My Voice and Showing Up For Me and You
Mental health is a sensitive topic. Lots of people nd it tough to discuss issues they face in this area.
You can make it a little easier for friends to open up and nd their voices by choosing your words carefully.
The right language communicates that you are supportive and caring, not judgmental, and encourages
people to be honest about what’s on their minds—or to ask for the help they need. Check out these tips
from the experts at the National Alliance on Mental Illness (NAMI) for talking about suicide and other
mental health challenges.
Your Language Matters

37
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation.
© 2023 Girl Scouts of the United States of America. All rights reserved.
Getting The Right Start
Senior and Ambassador (Grades 9-12) | Showing Up For Me and You
Right Start
Right Start
Getting the
YOU ARE
NOT ALONE
Getting help early can
keep you on the right track.
1. Rule out other physical health
conditions
2. Be honest about what you’re
feeling and be clear about
what you want
3. Ask for help fi nding a therapist
or mental health professional
that works for you
■ It can take some time to get an
appointment with a specialist,
so do not wait.
■ See if you can get an
appointment sooner by asking
or letting the specialist know if
you are in crisis.
■ While you wait, contact your
local NAMI for additional
supports and resources,
including the NAMI HelpLine
and support groups.
WORRIED?
U.S. youth
aged 6-17
ONE
SIX
IN
experience
a mental health
disorder each year.
Tell Someone
■ Family member
■ Close friend
■ Teacher or professor
■ Counselor or coach
■ Faith leader
WHAT
TO SAY
■ “I haven’t felt like myself lately,
and I don’t know what to do.
Can I talk to you about it?”
■ “I’m worried about stu that’s
going on right now, do you
have time to talk?”
■ “I’m having a really hard time;
will you go with me to see
someone?”
WHAT
TO DO
KEEP
IN MIND
Getting The Right Start
Supports Activity 3
If you are struggling with your mental health, it’s important to know that you are not alone. Lots of young people
face mental health and wellness challenges—so you should never feel embarrassed or worried about asking for help.
Show up for yourself with these tips from the experts at the National Alliance on Mental Illness (NAMI) on how to
get the conversation started.
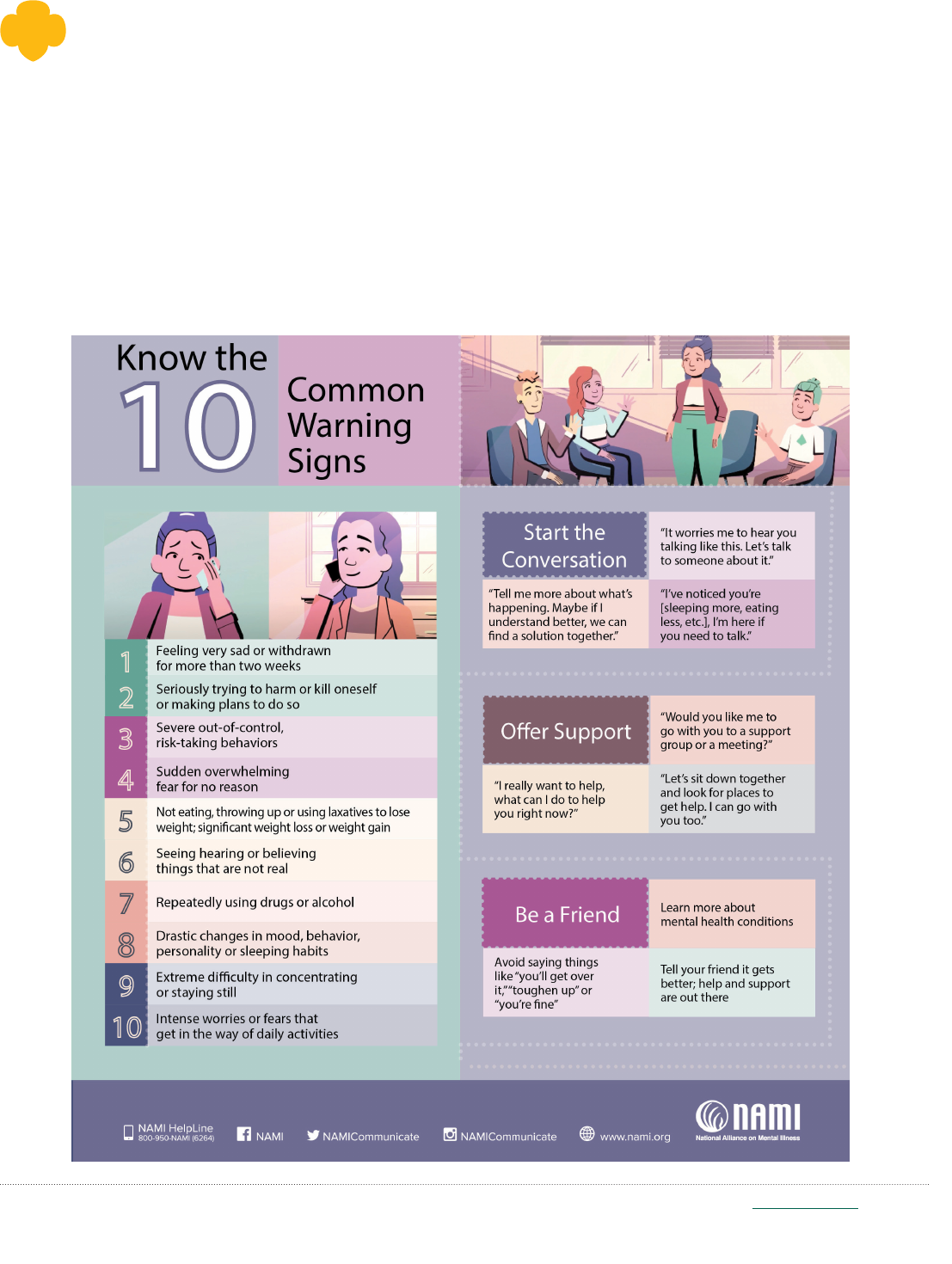
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation.
© 2023 Girl Scouts of the United States of America. All rights reserved.
Cadettes (Grades 6-8) | Finding My Voice
Senior and Ambassador (Grades 9-12) | Showing Up For Me and You
Help A Friend
How To Help A Friend
Supports Activity 3
Being helpful is part of the Girl Scout Promise and Law. Not only that, it’s a way of life. We all want to help our
friends! Unfortunately, even our closest pals don’t always tell us when they’re struggling. But there are some
clues that can tell you when someone is in trouble. Check out these tips from the experts at the National
Alliance on Mental Illness (NAMI) on how to recognize 10 common warning signs of serious problems—and
what you can do to help.
38
Detailed choice activities, meeting tools, and additional resources and materials can be found within the Volunteer Toolkit on my.girlscouts.org.
Made possible by HCA Healthcare Foundation.
© 2023 Girl Scouts of the United States of America. All rights reserved.
39
Senior and Ambassador (Grades 9-12) | Showing Up For Me and You
Active Listening Checklist
Active Listening Checklist
Supports Activity 4
Active listening is a skill that allows you to really hear and respond to what others are saying—not just their words,
but the feelings and thoughts that lie beneath them. It’s an important way to show up for yourself and others.
Active listening doesn’t just happen; it takes knowledge and practice. This checklist will help you to learn this
valuable skill.
Set yourself up so you can be focused.
Face toward the other person.
Do your best to maintain eye contact—but
take the other person’s cue. If they seem
uncomfortable keeping eye contact while
sharing, that’s okay!
Be mindful of your facial expressions. Try to
release judgment of what the other person is
sharing; convey your interest and concern.
When appropriate, nod to let the other person
know you hear them.
When appropriate, use encouraging words
like “yes,” “uh-huh,” “that makes sense,” or “I
would feel that way, too” to keep the
conversation going.
Pause to reflect on what you heard and process
it before you speak.
When appropriate, repeat what’s been said:
“What I'm hearing is...” or “Sounds like you
are saying...”
Ask questions when you need to: “What do you
mean when you say…?” “Can you say more about
that?” Give the other person a chance to clarify
but don’t challenge or speak for them.
Ask if they are looking for solutions or just
wanted to share. If they want it, brainstorm
solutions together. Together you can come up
with pros and cons for each to find one they feel
good about.
Interrupt or break in with your own thoughts;
allow the other person to nish before
chiming in.
Offer feedback. Do so only if the other person
asks for it or says it’s okay to do so.
Try to solve the problem. Ask rst before
offering a solution.
Be eager to share your own experiences. Instead,
support the person by letting them know
their problem matters and that they are being
heard—keep the focus on them.
Dismiss the other person’s issue as “not a big
deal” or by saying “You’ll get over it.” Make sure
you take their issue seriously.
Use “should,” as in “You should do x, y, or z.”
We don’t necessarily know what is best for
someone else.
Offer advice just because the other person
wants it. If you don’t know what to say, it’s okay
to say you’re not sure what to do. Help them
nd someone or somewhere that will, such as a
trusted adult.
Do Don't
